Plantar fasciitis is one of the most common causes of heel pain. Caused by inflammation of the plantar fascia, a thick, web like band of tissue that runs across the bottom of your foot and connects your heel bone to your toes, helping you walk. Your plantar fascia ligaments experience a lot of wear and tear in day-to-day life. Too much pressure on your feet can damage or tear the ligaments.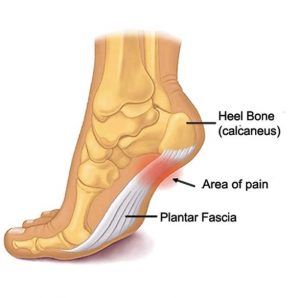
Plantar fasciitis usually causes a stabbing sensation that typically occurs with your first steps of the day. Pain usually decreases as you get up and move but may return after extended periods of standing or sitting.
The condition more common in runners, people who are overweight and those that wear shoes with insufficient support. You can usually ease the pain yourself, however if the pain does not improve within 2 weeks speak to your doctor.
Symptoms of Plantar Fasciitis
The primary complaint of plantar fasciitis is a stabbing pain at the bottom of the heel or sometimes at the bottom mid-foot area. It typically affects one foot, but it can affect both feet.
Pain progresses gradually over time. The pain can be dull or sharp with some people feeling a burning or ache on the bottom of the foot. The pain is generally worse in the morning when you take your first steps out of bed, or if you have been sitting or lying down for an extended period.
After physical activity and exercise, the pain can intensify due to increased irritation or inflammation. Usually you will not feel the pain during the activity, but rather after stopping.
Causes of Plantar Fasciitis
Your plantar fascia is shaped like a bowstring, supporting the arch of your foot and absorbing shock when you walk. If strain and tension on the bowstring becomes too much, small tears can occur in the fascia.
Plantar fasciitis is caused by straining your plantar fascia. It is not always clear why this occurs. Risk factors that can increase your chance of developing plantar fasciitis:
- Wearing inappropriate shoes with poor cushioning or support.
- Obesity or being overweight increases pressure on your plantar fascia ligaments.
- Age. People between the ages of 40 and 70 are at a higher risk of developing the condition.
- Gender. Women that are pregnant often experience bouts of plantar fasciitis, particularly in late pregnancy.
- Certain types of exercise. Taking part in physical activities such as dancing or long distance walking or running.
- Occupation. An active job that involves being on your feet for long periods, such as working in a factory or hairdresser.
- Structural foot problems. High arches, tight Achilles tendons or flat feet may increase your chance of developing the condition.
Diagnosis of Plantar Fasciitis
In order to diagnose plantar fasciitis, your doctor will take a full medical history and carry out a physical examination. During the exam, your doctor will look for areas of tenderness in your foot. They may ask you to flex your foot as they push on the plantar fascia to assess whether the pain increases. The pain location will help determine the cause.
Ordinarily no imaging tests are required. Your doctor might suggest an X-ray or magnetic resonance imaging (MRI) to eliminate the possibility of other foot problems such as a bone fracture.
Treatment
In the majority of cases, people who experience plantar fasciitis recover over the course of several months using conservative treatments such as resting, icing the affected area and stretching. Over the counter pain relievers such as ibuprofen may help ease the pain and inflammation caused by plantar fasciitis.
Stretching and strengthening exercises or using specific devices can help relieve symptoms. Therapies include:
Physical therapy
You may be shown how to apply athletic taping to support the bottom of your foot. A physical therapist can also show you a sequence of exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles.
Night splints
Your doctor or physical therapist might suggest that you wear a splint that stretches your calf and the arch of your foot while you sleep. This secures the plantar fascia and Achilles tendon in a lengthened position overnight to encourage stretching.
Orthotics
To help distribute pressure to your feet more evenly, your doctor might prescribe off-the-shelf or custom-fitted arch supports (orthotics).
If more-conservative measures fail to work after several months, your doctor may suggest:
Injections
Injecting steroid medication into the affected area can offer temporary pain relief. Multiple injections are not recommended as they can weaken your plantar fascia and possibly cause it to rupture.
Extracorporeal Shockwave Therapy (EWST)
A non-invasive procedure where soundwaves are directed at the area of heel pain to increase blood flow and stimulate healing. EWST is typically used for chronic plantar fasciitis. Treatment sessions are short and 2 or 3 sessions will usually be required.
Surgery
In some cases, you may need surgery to detach the plantar fascia from the heel bone. Surgery is only an option when the pain is severe or lasts more than 6-12 months and other treatments have failed. Surgery can be carried out as an open procedure or through a small incision.
Plantar Fascia Release Surgery
If you have a standard range of motion in your ankle and persistent heel pain, your doctor may recommend a partial release procedure. This is an outpatient surgery that takes 15-20 minutes to perform and can be done with general anaesthetic. During fascia release surgery, the plantar fascia ligament is partially cut to relieve tension. Any large bone spurs will be removed at the same time. Although the surgery can be performed using keyhole surgery, it can be more difficult than with an open incision.
Open Surgery
If your doctor has suggested open surgery, they will start by cutting a small area at the bottom of your foot in order to operate with the plantar fascia ligament exposed. They will aim to relieve the tension on your plantar fascia by detaching it from the heel bone, removing heel spurs, releasing trapped nerves or removing scar tissue.
Recovering from Plantar Fasciitis
For most people, plantar fasciitis improves within a few months of home treatments. These include resting, icing, and stretching. You can also help your plantar fascia recovery by stabilising your foot with tape. This limits movement in the ligament can move.
You can use zinc oxide tape or kinesiology tape. It may take some practice, but you can tape your foot yourself and help aid the recovery process.
Risks and Complications
Ignoring the condition can lead to chronic heel pain, arch pain and scar tissue. This can change the way you walk and injure your legs, knees, hips and back. Steroid injections can weaken the plantar fascia ligament and cause potential rupture of the ligament.
With surgery, there is always a risk of complications such as:
- Bleeding or blood clots
- Infection
- Reactions to the anaesthetic
- Nerve damage
Outlook
In most cases, you will not need surgery to ease the pain. The condition can improve through physical therapy, home remedies, and medical treatments. However, treatment can take several months to 2 years to improve your symptoms and surgery should be regarded as a last resort option.
Need Help?
If you are experiencing pain in your foot and you think it could be plantar fasciitis, you can be seen by a Consultant Orthopaedic Foot and Ankle Surgeon at One Ashford Hospital, usually within 48 hours. One Ashford Hospital is well placed to see patients with knee injuries from Ashford, Maidstone, Canterbury, Folkestone, Dover and all surrounding villages. To book an appointment, call the hospital direct on 01233 364 022 or email here.


 One Ashford
One Ashford One Hatfield
One Hatfield